Anal Fistula
An anal fistula is a quite common disorder of the area of the anus, which if neglected can have serious complications and even be life-threatening.
Modern and minimally invasive techniques are used to treat anal fistulas depending on their location.

What is an Anal Fistula?
Anal fistulas constitute abnormal communication channels between the intestine and the skin around the anus.
Why choose Dr. Konstantinidis?
Dr. K. M. Konstantinidis and his team possess vast experience in the field of laparoscopic and robotic surgery.
Dr. Konstantinidis is the pioneer of Robotic Surgery in Greece and one of the leading figures internationally in the field, having performed the largest series of General Surgery operations in Europe with the innovative Da Vinci® robotic system, including inguinal hernia surgeries.
What are the symptoms of Anal Fistulas?
The main signs and symptoms of an anal fistula include pain, redness and swelling in the anal area.
Also, it is usually manifested by the outflow of pus through the fistula tract to the skin.
As a secondary consequence of anal fistula, anal itching, or skin lesions due to the secretion of pus from the fistula are observed.
What causes Anal Fistulas?
Usually, anal fistulas form as a result of untreated anal abscesses. Abscesses are caused by inflammation following the blocking of the perianal glands.
When such an abscess is formed, the body tends to drain the pus to the skin around the anus, thus forming an anal fistula.
Also, anal fistulas may be caused as a result of other, less common conditions, such are:
- Crohn’s disease
- Radiotherapy
- Injury
- Sexually transmitted diseases
- Tuberculosis
What are the complications of Anal Fistulas?
If treatment for an anal fistula is delayed and the latter is allowed to worsen, there is a risk that this will lead to perineal gangrene and systemic sepsis, a condition that may even be threatening to the patient’s life.
How are Anal Fistulas diagnosed?
As a rule, the diagnosis is made during the clinical examination of the area around the anus by a physician.
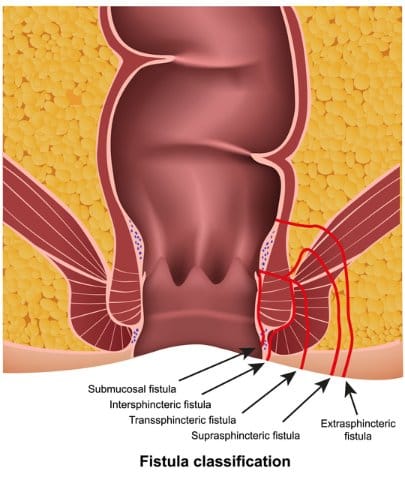
After detecting the fistula, the physician aims to determine its depth and the course of its tract.
Additional tests will almost always be required, such as:
- endoscopic examination of the anus and rectum
- colorectal ultrasound and / or magnetic resonance imaging (MRI)
The detection of a fistula may be accompanied by further tests, such as a colonoscopy, to determine if the patient has Crohn’s disease. About 25% of people with Crohn’s disease develop anal fistulas.
How are Anal Fistulas treated?
The treatment of anal fistulas is always surgical.
Basic principles of anal fistula treatment include:
- detecting and destroying the inner mouth of the fistula
- locating the course of the tract and excising it completely along its entire length
- cutting as less as possible through the sphincter
The application, by a specialized surgeon, of one of the existing methods for the treatment of hemorrhoids, fissures and perianal abscesses and fistulas offers excellent and permanent results.
The Surgical Team of Dr. Konstantinidis applies minimally invasive methods for the treatment of anal fistulas, such as FiLaC (Fistula tract – Laser – Closure), LIFT (Ligation of the Intersphincteric Fistula Tract) and VAAFT (Video-Assisted Anal Fistula Treatment).
Anal fistula removal of using Laser (FILAC), Seton, Fibrin Glue, Plug, LIFT technique
FiLaC method
The FiLaC method includes the use of therapeutic laser for the treatment of the fistula avoiding the injury of the sphincter and the neighboring muscles, thus minimizing the risk of incontinence.
Seton Techniques
The seton is a piece of surgical thread that is left in the fistula for several weeks to keep it open.
This helps the fistula to drain and as a result to heal, thus avoiding unnecessary injury to the sphincter muscles.
LIFT technique
LIFT technique is used for the treatment of fistulas that penetrate the sphincter muscles, which should not be cut off.
During treatment, an incision is made in the skin above the fistula and the sphincter muscles are placed aside.
The fistula is then sealed at both ends and left open to heal.
Fibrin glue
Using biomaterials such fibrin glue for the treatment of anal fistulas is currently the only non-surgical option.
The surgeon injects the fibrin glue which in turn seals the fistula and helps it heal.
It is generally less effective than more invasive approaches but may be a useful option for fistulas that penetrate the anal sphincter muscles.
Plug
Another option for treating fistulas is to insert a bioprosthetic plug.
It refers to a cone-shaped plug made of animal tissue that is used to block the internal opening of the fistula.
Endoscopic treatment of anal fistula (VAAFT)
What is Video-assisted Anal Fistula treatment (VAAFT)?
Endoscopic treatment of peripheral fistulas using video (VAAFT) is a new, minimally invasive technique for the treatment of complex peripheral fistulas.
The main feature of this technique is the ability to use video endoscopic technology for accurate imaging of the anatomy of the fistula and its pathways, while maintaining the function of the sphincter, resulting in minimal complications and faster recovery.