Duodenal cancer
Duodenal cancer is one of the rarest and most aggressive forms of malignancy.
However, despite the aggressiveness of the disease, the treatment of duodenal cancer shows high success rates when treated by experienced and specialized surgeons.
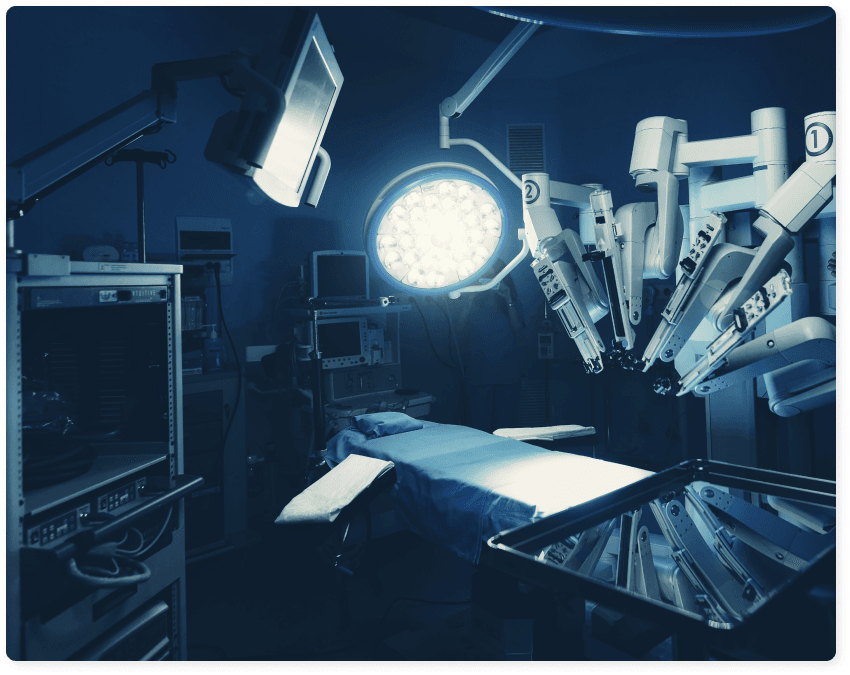
Dr. Konstantinidis and his Surgical Team constitute a reference point in Greece for the treatment of duodenal cancer, performing Robotic Surgery, with the state-of-the-art da Vinci Xi robotic system, at Athens Medical Center.
Since 2006, when the Robotic Surgery program began at Athens Medical Center, Dr. Konstantinidis and his Surgical Team have performed a large number of robotic surgeries to treat duodenal cancer, with excellent success rates, ensuring optimal oncological outcomes and minimizing the risk of complications, even with the most difficult of cases.
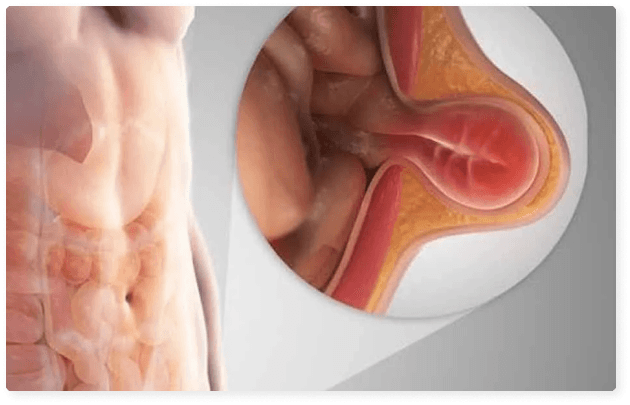
What is the Duodenum?
The duodenum is the first and smallest part of the small intestine, is C-shaped and surrounds the head of the pancreas.
The duodenum is responsible for processing the acid produced by the stomach to aid digestion.
This acid is mixed with alkaline fluids produced by the pancreas and bile to achieve digestion and absorption of nutrients in the subsequent parts of the small intestine (jejunum and ileum).
What is Duodenal Cancer?
Duodenal cancer is a malignancy that develops in the first part of the small intestine that follows the stomach into the digestive tract.
Among all cancers of the small intestine (jejunum, duodenum and ileum), duodenal cancer comes in second place in terms of frequency, after cancer of the ileum.
The most common type of duodenal cancer is adenocarcinoma.
Θέλεις να μάθεις περισσότερα για Duodenal cancer ;
Λάβε το infographic στο email σου
Why choose Dr. Konstantinidis?
Dr. K. M. Konstantinidis and his team possess vast experience in the field of laparoscopic and robotic surgery.
Dr. Konstantinidis is the pioneer of Robotic Surgery in Greece and one of the leading figures internationally in the field, having performed the largest series of General Surgery operations in Europe with the innovative Da Vinci® robotic system, including inguinal hernia surgeries.
What Are The Symptoms Of Duodenal Cancer?
Usually, duodenal cancer has no symptoms in the early stages of the disease and is therefore difficult to diagnose in time.
When cancer cells begin to form in the duodenum, the tumor that forms can block the passage (blockage) of food through the digestive system.
When food is prevented from passing through the small intestine or when the body is no longer able to absorb the necessary nutrients from food, then symptoms appear such as:
abdominal pain
weakness and / or fatigue
nausea and / or vomiting
constipation
gastroesophageal reflux
weight loss
blood loss
jaundice
In most cases, the symptoms appear in the later stages of the disease as soon as the tumor grows large enough to block the passage of food. At this point, a mass in the abdomen may be observed.
What are the risk factors for Duodenal Cancer?
The risk factors for duodenal cancer have not yet been adequately identified.
However, there are suspicions that diet plays a role in the onset of the disease. A diet rich in pastries, pasta, processed sugar and red meat is generally a risk factor for small bowel cancer and may therefore contribute to duodenal cancer.
Alcohol and coffee consumption as well as smoking can also increase the risk of developing the disease.
How is Duodenal Cancer Diagnosed?
Diagnosis is the first step in treating the disease. There are many advanced diagnostic methods that can help diagnose duodenal cancer, such as:
- Barium meal with x-ray
- Upper gastrointestinal endoscopy to detect abnormal cells
- Tissue sample biopsy
- Intra-abdominal ultrasonography
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Endoscopic Ultrasound (EUS), through the stomach, which allows the physician to obtain “core biopsies” from the tumor
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Positron Emission Tomography (PET), in specific cases
EUS and ERCP are commonly used to substantiate imaging findings, while also contributing significantly to the detection of early cancers.
How is Duodenal Cancer Treated?
The treatment of duodenal cancer depends on the type, location and size of the tumor, as well as the extent of the disease.
The treatment plan is formed after consultation of the treating physicians from all relevant specialties (General Surgeon, Oncologist, Pathologist, etc.) within the Oncology Board, convened for each patient.
Surgery is usually the main treatment for this type of cancer, assisted sometimes by chemotherapy and/or radiotherapy, and it involves removing parts of the affected duodenum.
However, caution is required when removing tumors due to the proximity of the duodenum to the pancreas, bile duct and other important organs, such as the liver and spleen.
That is why the surgical treatment of the disease shows high success rates, when performed by experienced and qualified surgeons.
- Two types of surgery are commonly performed to treat duodenal cancer:
- Partial duodenectomy, which involves the removal of the affected part of the duodenum -as well as the adjacent tissues- and the subsequent anastomosis of the small intestine
- Whipple’s procedure, which involves removing the head of the pancreas, a small terminal part of the stomach, duodenum, gallbladder and common bile duct
Both operations can be performed with open surgery or minimally invasive techniques, i.e. laparoscopic surgery, or robotic surgery, which is an evolution of laparoscopy and combines optimal oncological outcomes with the least possible risk of complications.
Duodenectomy
Laparoscopic Partial Duodenectomy
What is Laparoscopic Partial Duodenectomy?
Laparoscopic partial duodenectomy is a procedure that minimizes injury to tissues such as muscles, nerves and blood vessels and involves the removal of a part of the small intestine, the duodenum, affected by cancer and adjacent tissues, as well as the anastomosis of the remaining healthy parts of the organ.
During the laparoscopic partial duodenectomy, the surgeon inserts the special, thin laparoscopic tools through 4-5 small holes. One of these tools is the laparoscope, a tiny telescope with a video camera attached that allows the surgeon to view the patient’s internal organs at a magnified screen.
What are the advantages of Laparoscopic Partial Duodenectomy?
As a minimally invasive technique, laparoscopic partial duodenectomy has many important advantages over open surgery, such as:
- Minimal blood loss and postoperative pain
- Faster recovery and return of the patient to daily activities
- Shorter hospital stay
- Minimization of trauma-related complications (perforation, rupture, hernia, chronic pain), but also respiratory and cardiovascular complications
- Elimination of postoperative adhesions
- Optimal cosmetic outcome
When is Laparoscopy not preferable?
Laparoscopic partial duodenectomy may not be possible in a very small number of patients. Factors that may increase the chances of having open surgery are obesity, a history of previous multiple operation on the abdomen, which may have caused many adhesions, bleeding problems during surgery, and the inability to get a clear picture of the organs.
Dr. Konstantinidis and his Surgical Team have vast experience in laparoscopic duodenectomy, both total and partial, having performed hundreds of surgeries since 1991.
Laparoscopic surgery converts to open in no more than about 1-2% of the cases and is usually associated with problems of the patient’s anatomy.
Robotic Partial Duodenal resection
What is Robotic Partial Duodenal Resection?
Robotic partial duodenectomy is an evolution of the laparoscopic technique and it involves the removal of the part of the duodenum that bears the tumor, as well as the tissues around it, with the help of a state-of-the-art robotic system that allows the surgeon to have:
- better view and access to the tumor, as well as
- unsurpassed accuracy and flexibility of movements
The surgeon is seated on a console through which he has visual contact with the surgical field in 3D and largely magnified, while navigating the robotic arms with the special, robotic tools that resemble the laparoscopic ones.
What are the advantages of Robotic Partial Duodenectomy?
Robotic partial duodenectomy maintains all the advantages of the laparoscopic technique over open surgery and offers the following on top:
- High-definition 3D color and still image, which gives the feeling that the surgeon’s eyes and hands are inside the patient’s body
- Minimal intervention in the patient’s body with incisions not exceeding 0.8 cm
- Maximum flexibility of tools and precision of movements at the level of a millimeter by eliminating the natural trembling of the hands
- Avoidance of injury to important intra-abdominal organs, such as the spleen, liver, bile ducts, etc., as the movements of the robotic arms are stable and precise
- Great ease and accuracy in suturing the intestinal anastomoses, i.e. the reunifying of the intestine after duodenal resection
- Less physical fatigue of the surgeon (operates sitting on the console), which can make the difference in long surgeries
- Ability to operate even on overly obese individuals (Body Mass Index> 60) due to the stability of robotic tools against increased intra-abdominal and wall pressures
- Extensive resolution of adhesions in patients with previous open abdominal operations
- Low pneumoperitoneum pressure during surgery resulting in reduced postoperative pain and of carbon dioxide concentration in the blood
- Easy identification and maintenance of important pelvic nerves, so as not to affect the function of urination and sexual activity in the lower anterior duodenectomy
Bloodless removal of all or part of the affected intestine
What happens after Robotic Partial Duodenectomy?
After the robotic partial duodenectomy the patient may stand up and walk the next day with minimal postoperative pain.
The intestine resumes its proper function soon, in 2-4 days, when the feeding with soft food begins.
The patient is discharged from the hospital in a few days and is ready to return to his daily activities in about 1-2 weeks, avoiding lifting weights for a while.